Pancreatitis
What is Pancreatitis?
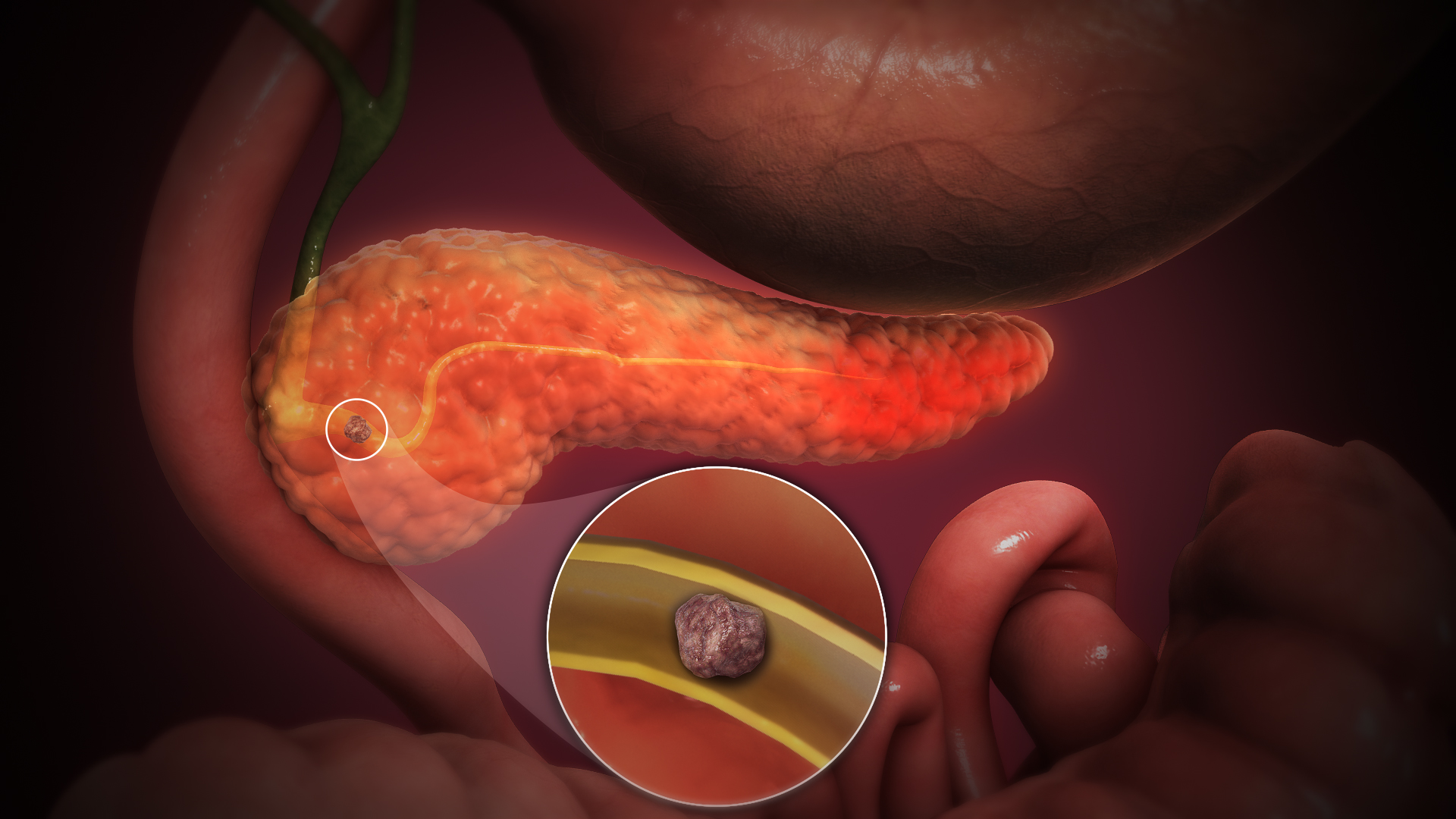
Pancreatitis is an inflammation of the pancreas, a vital organ responsible for digestion and regulating blood sugar levels. This condition can be acute, occurring suddenly and lasting for a short period, or chronic, developing over time and leading to long-term complications.
Types of Pancreatitis
There are two main types of pancreatitis:
- Acute Pancreatitis: A sudden inflammation that can be life-threatening if not treated promptly. Common causes include gallstones, alcohol consumption, and certain medications.
- Chronic Pancreatitis: Long-lasting inflammation that can result in permanent damage to the pancreas. It is often associated with prolonged alcohol use and other underlying health conditions.
Symptoms of Pancreatitis
The symptoms of pancreatitis can vary based on the type and severity of the condition but typically include:
- Severe abdominal pain that may radiate to the back
- Nausea and vomiting
- Fever and rapid pulse
- Swollen and tender abdomen
- Jaundice (yellowing of the skin and eyes)
Recognizing these symptoms early is crucial for effective treatment.
Causes of Pancreatitis
Common causes of pancreatitis include:
- Gallstones: These can block the pancreatic duct, leading to inflammation.
- Alcohol use: Chronic alcohol consumption is a significant risk factor for both acute and chronic pancreatitis.
- Medications: Certain medications can trigger inflammation in the pancreas.
- Genetic factors: Some individuals may have a genetic predisposition to pancreatitis.
Diagnosis of Pancreatitis
To diagnose pancreatitis, healthcare providers may perform:
- A thorough medical history review and physical examination.
- Blood tests to check for elevated levels of pancreatic enzymes.
- Imaging tests such as CT scans or ultrasounds to assess the pancreas and surrounding organs.
Treatment Options for Pancreatitis
1. Initial Management
For acute pancreatitis, initial treatment usually involves:
- Hospitalization: Severe cases may require hospitalization for monitoring and treatment.
- Fasting: Patients may be advised to avoid food and drink for a few days to allow the pancreas to heal.
- Pain management: Medications to control pain and discomfort.
2. Long-Term Management
For chronic pancreatitis, ongoing management may include:
- Dietary changes: A low-fat diet that includes small, frequent meals can help manage symptoms.
- Enzyme replacement therapy: Supplements to aid digestion if the pancreas is not producing enough enzymes.
- Lifestyle modifications: Avoiding alcohol and smoking, and maintaining a healthy weight.
3. Surgical Options
In certain cases, surgery may be necessary to:
- Remove gallstones or blockages.
- Drain fluid collections or cysts.
- Perform a pancreatic resection for severe chronic pancreatitis.
Finding a Pancreas Specialist in Your Area
If you’re looking for a pancreas specialist in Mulund, Mumbra, and Bhiwandi, it’s important to consult a healthcare provider with expertise in gastrointestinal disorders. A specialist can offer a comprehensive evaluation and develop a personalized treatment plan to effectively manage your condition.
Conclusion
Pancreatitis can significantly impact your health and quality of life. By understanding the causes, symptoms, and treatment options available, you can take proactive steps toward better management. If you’re experiencing symptoms of pancreatitis, don’t hesitate to seek help from a qualified pancreas specialist in Mulund, Mumbra, and Bhiwandi for expert guidance and support.